Eczema concerns?
Get instant expert guidance with our smart AI platform.
Join NowEczema, or atopic dermatitis, is one of the most common chronic skin conditions in the world—yet access to treatment remains far from equal. Millions of people worldwide suffer from severe itching, inflammation, sleep disruption, and psychological distress due to untreated or under-treated eczema. But what if care wasn’t limited by cost, location, or insurance status?

In 2025, universal health coverage (UHC) has become a central focus of global health equity. And when it comes to chronic skin diseases like eczema, UHC could be the key to closing treatment gaps, reducing health disparities, and ensuring every patient has access to quality, continuous care.
This article explores the critical relationship between universal health coverage and eczema—and what needs to change to make skin health a basic human right, not a privilege.
Universal health coverage means that everyone, everywhere can access essential health services—from prevention and diagnosis to treatment and rehabilitation—without suffering financial hardship.
It’s a key target of the World Health Organization’s Sustainable Development Goals (SDG 3.8) and includes:
Yet, nearly half the global population lacks full coverage, and even in wealthy nations, gaps persist—especially in dermatology.
Eczema affects approximately 230 million people worldwide and is especially common in children, though many continue to suffer well into adulthood. While it may appear to be a minor skin issue, untreated eczema can lead to:
According to the Global Burden of Disease Study, eczema ranks among the top 10 non-fatal diseases impacting quality of life, particularly due to its psychosocial toll and chronic nature.
And yet—eczema is often underdiagnosed, undertreated, or simply not prioritized within public health systems.
In countries without universal healthcare—or for individuals without insurance—eczema patients face steep barriers:
For example, dupilumab (Dupixent)—a breakthrough biologic treatment for moderate-to-severe eczema—can cost over $3,000/month without coverage. That’s out of reach for most people.
Even basic necessities like hypoallergenic moisturizers, prescription topicals, or teledermatology access can be financially burdensome.
When eczema is covered by a robust health system, outcomes improve dramatically. Countries with UHC frameworks such as Sweden, Japan, and the UK often see:
A 2022 cross-national study published in Global Atopic Dermatitis Atlas found that access to subsidized dermatological care directly correlated with reduced eczema severity and flare frequency across multiple OECD countries.
Moreover, universal coverage enables preventive care—helping patients manage triggers, build effective routines, and avoid expensive complications down the line.
As of 2025, several countries have made notable strides:
But gaps remain. In the U.S., for example, many Medicaid plans do not fully cover dermatology or biologics, leaving vulnerable patients with few options. And in low-income countries, dermatology is often concentrated in cities, with rural patients facing hours of travel or no access at all.
Despite its high prevalence, eczema and other chronic dermatologic conditions are often excluded from national health priorities. This is a mistake. Skin diseases:
In other words, eczema isn’t just about comfort—it’s about systemic health. Ensuring access to care can improve school attendance, workforce productivity, and healthcare efficiency.
Skin is the largest organ in the body—and it’s time we treated it as such.
Whether you’re an eczema patient, caregiver, or healthcare provider, here are ways to advocate for change:
Not necessarily. UHC means that essential care is affordable and accessible, often through a combination of public insurance, subsidies, and regulated pricing.
Because it’s non-fatal and often invisible, eczema can be dismissed as cosmetic. Advocacy and education are crucial to reframing it as a serious immune and inflammatory condition.
Absolutely. Teledermatology expands reach into rural and underserved areas, offering faster diagnosis, continuity of care, and less strain on physical clinics.
At its core, universal health coverage and eczema care are about one thing: dignity. Everyone deserves relief from pain, sleep loss, and the psychological weight of chronic illness—no matter where they live or how much they earn.
Improving access to eczema treatment is a public health priority, and one that pays dividends in productivity, equity, and well-being. As we move toward a more inclusive and sustainable future, let’s make sure skin health isn’t left behind.
For daily support between doctor visits, NellaDerm’s dermatologist-designed skincare offers barrier-restoring, eczema-friendly products that are accessible, evidence-based, and designed with sensitive skin in mind.
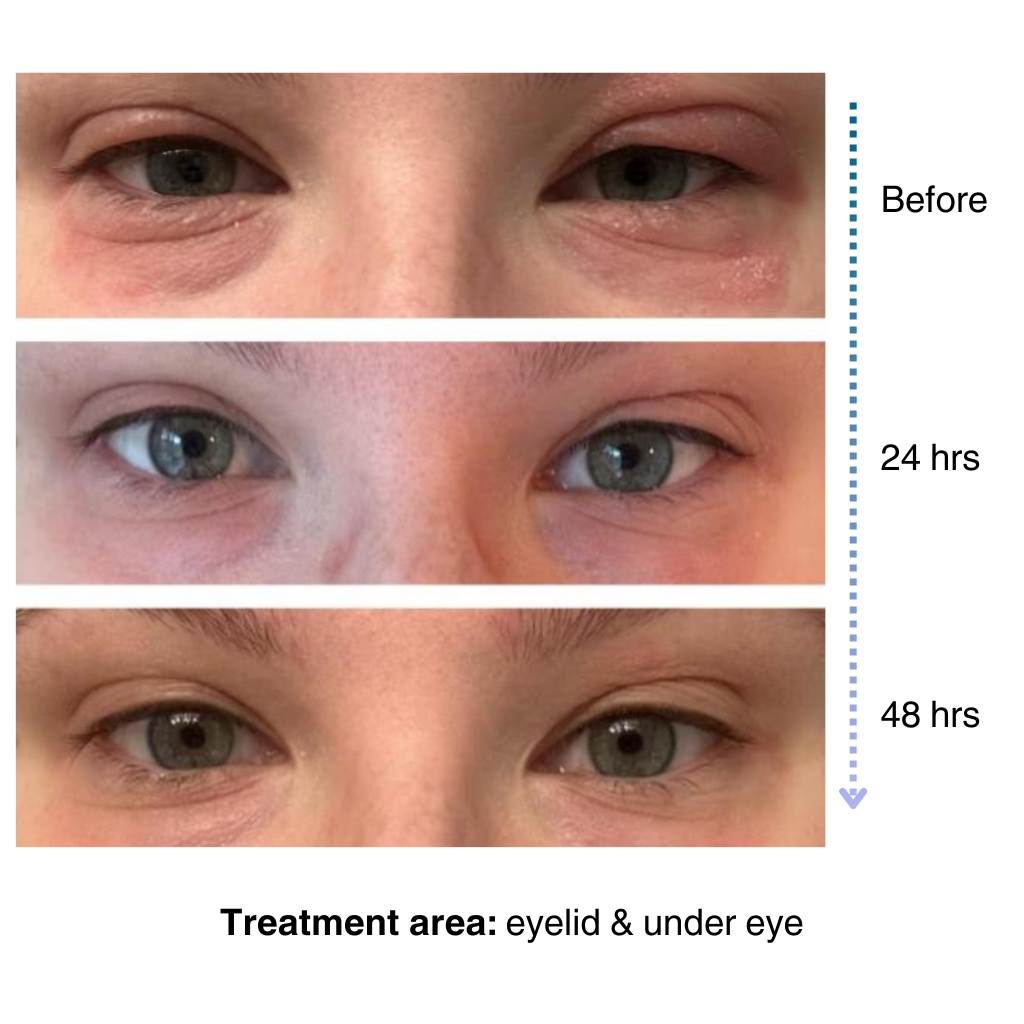
It’s easy to apply and isn’t chalky at all. I’ve been applying it multiple times a day… I’ve tried multiple new products to try and treat my eye eczema, and this is definitely the best I’ve tried so far.
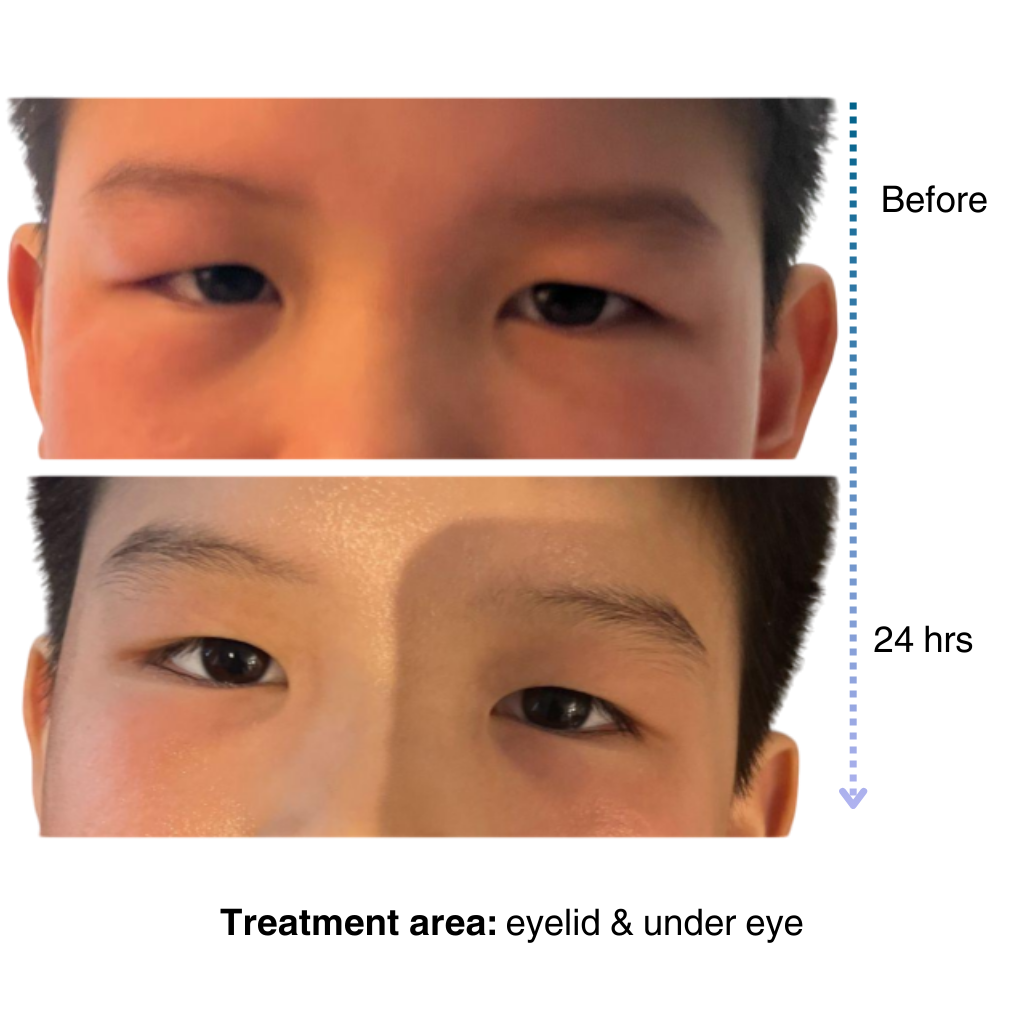
My 7-year old son has been dealing with eczema on his face for a long time, and it’s been so tough to find something that really works…..I’m amazed by the results! Within one day, the redness and rough patches on his face significantly improved…. he doesn’t mind using it at all because it doesn’t sting or feel greasy. – Lily


Like many of you, our eczema journey is personal. That’s why we’re committed to creating a space for the eczema community to share experiences, be empowered through evidence-based solutions, and learn practical tips for daily life.
– Sajjad, Founder & CEO of NellaDerm
