Eczema concerns?
Get instant expert guidance with our smart AI platform.
Join NowFor decades, bacteria have been cast as the enemy in skincare. From harsh cleansers to antibacterial soaps, we’ve built an entire culture around eliminating microbes. But science is rewriting the script, and this time, bacteria might just be the heroes.
Welcome to the future of eczema care: bacteria therapy. Known formally as microbiome-based therapy, this cutting-edge approach is transforming how we treat chronic skin conditions by restoring balance, not destroying it.
In this post, we explore the exciting link between bacterial therapy and eczema, how your skin microbiome works, and what 2025’s most promising research says about using good bugs to soothe inflammation and rebuild your skin’s natural defenses.
Your skin isn’t just a barrier, it’s home to trillions of microorganisms, including bacteria, fungi, and viruses. Together, they form the skin microbiome, an ecosystem that helps:
In healthy skin, this ecosystem is diverse and balanced. But in eczema, that balance is often disrupted—especially by the overgrowth of one common bacterium: Staphylococcus aureus (S. aureus).
A 2022 NIH paper confirmed that eczema-prone skin shows significantly reduced microbial diversity, with pathogenic species like S. aureus dominating and driving inflammation.
Bacteria therapy—sometimes called live biotherapeutic treatment or topical probiotic therapy—involves introducing beneficial bacteria to the skin to rebalance the microbiome.
Rather than wiping everything out (as with antibiotics), bacterial therapy selectively encourages helpful microbes that:
These “good bugs” act like peacekeepers—restoring order in the skin’s microscopic community.
Many therapies use Staphylococcus hominis or Roseomonas mucosa, two bacteria known to suppress S. aureus growth. By restoring competition, these microbes naturally limit flare triggers.
Certain microbes help produce ceramides and other lipids that repair the stratum corneum—the outermost skin layer. This makes skin less prone to cracking, dryness, and allergen penetration.
Research shows that some commensal bacteria modulate immune pathways, reducing levels of inflammatory cytokines (like IL-4 and IL-13) commonly seen in eczema.
By stabilizing the microbiome, bacterial therapy may help the skin respond more calmly to environmental stressors, allergens, or friction, reducing overall flare intensity.
Bacteria therapy may sound futuristic, but it’s already showing real promise in clinical studies.
While still emerging, bacterial therapy for eczema is now being developed in several delivery formats:
Some dermatology clinics even offer microbiome assessments, using skin swabs to customize therapy based on your unique microbial makeup.
Please note these treatments are still in clinical phases. Always consult your dermatologist before trying over-the-counter “probiotic skincare” not backed by clinical trials.
As bacterial therapy evolves, the next frontier lies in precision dermatology. That means:
Think of it as a probiotic prescription for your skin, tailored like a fingerprint. In time, this could replace long-term steroid use and dramatically reduce flare recurrence.
While prescription bacterial therapy may still be on the horizon for most, there are steps you can take now to nurture your microbiome and support future treatment success:
These strip away good microbes. Use gentle, pH-balanced, fragrance-free cleansers.
Dry skin impairs microbial diversity. Choose non-comedogenic, microbiome-friendly moisturizers.
NellaDerm’s eczema-friendly moisturizers are formulated to support barrier health and reduce microbiome disruption.
Look for skincare with prebiotic ingredients like inulin or oat extract, which feed beneficial bacteria and promote balance.
Only use antibiotic ointments under medical supervision. Overuse can lead to resistant bacteria and microbiome damage.
Read more about the microbiome in our recent blog post.
Not exactly. Probiotics refer to live bacteria you ingest. Bacteria therapy for eczema involves topical application of specific skin-compatible strains designed to rebalance your microbiome.
No—these aren’t formulated for skin and could cause infections or irritation. Always use dermatology-approved products or participate in clinical studies under supervision.
Many treatments are in Phase II or III trials, so broader availability could come within 1–3 years. Keep an eye on clinical updates and talk to your dermatologist about future options.
The relationship between bacteria therapy and eczema marks one of the most promising shifts in dermatology today. By moving from suppression to symbiosis, we’re entering a new era of healing—one that embraces the skin’s natural intelligence and empowers patients with long-term, side-effect-free solutions.
Until prescription therapies arrive, focus on protecting your skin microbiome with gentle, evidence-backed care. For barrier-supportive skincare designed with your microbiome in mind, visit NellaDerm.com and discover what your skin can do when it’s finally in balance.
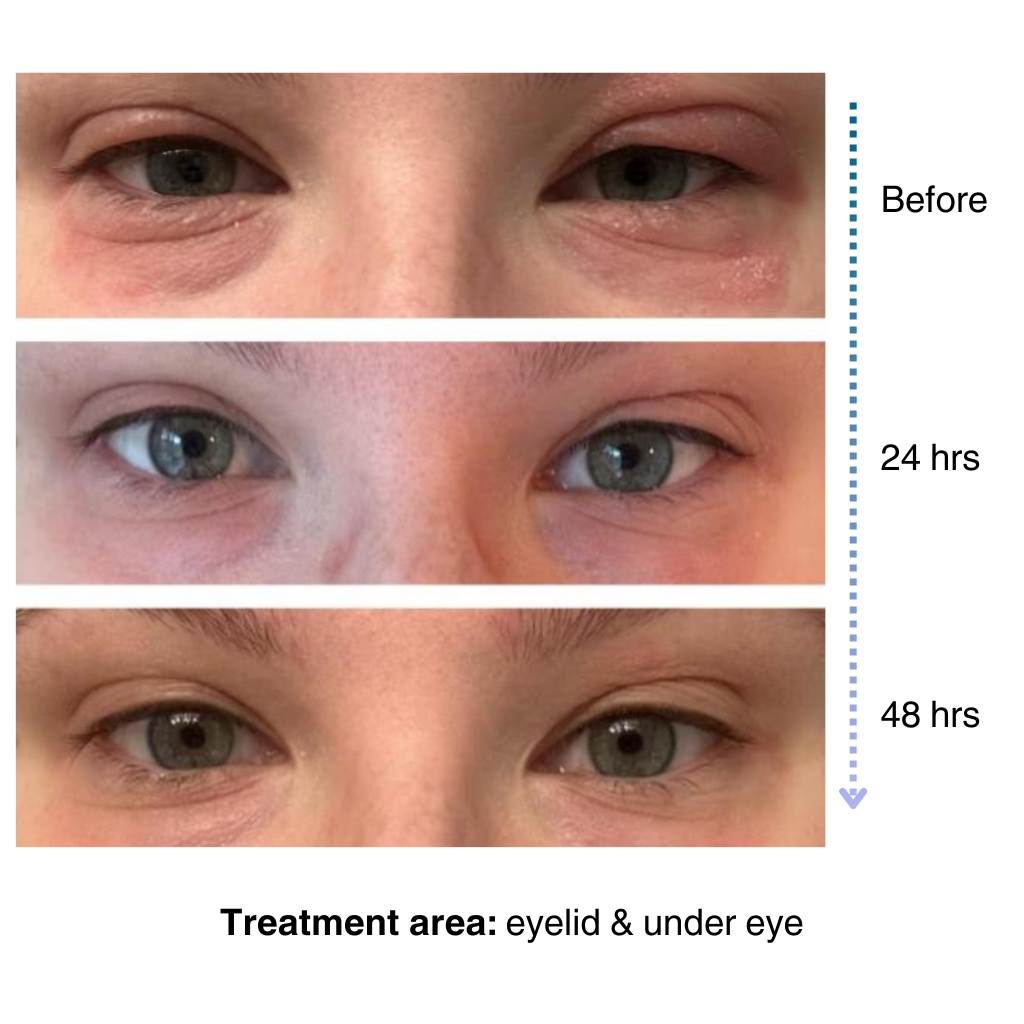
It’s easy to apply and isn’t chalky at all. I’ve been applying it multiple times a day… I’ve tried multiple new products to try and treat my eye eczema, and this is definitely the best I’ve tried so far.
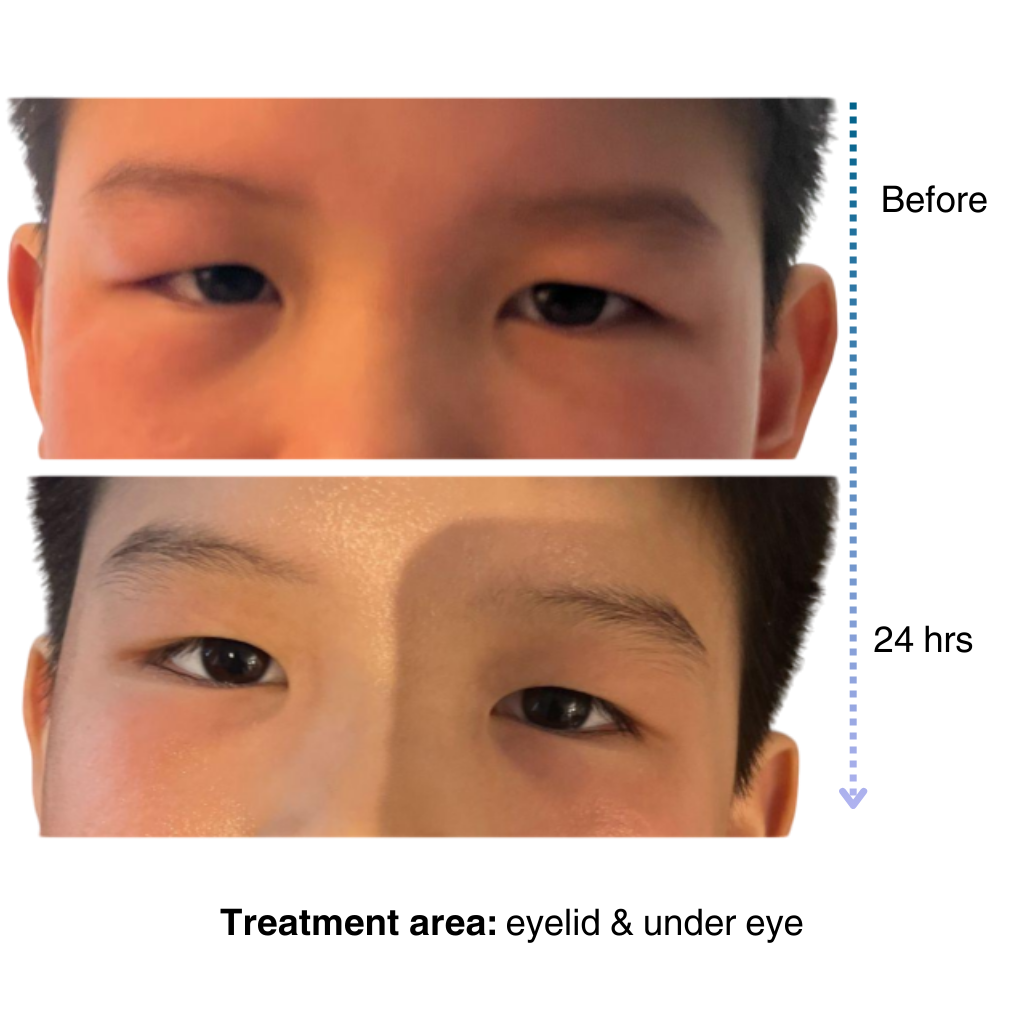
My 7-year old son has been dealing with eczema on his face for a long time, and it’s been so tough to find something that really works…..I’m amazed by the results! Within one day, the redness and rough patches on his face significantly improved…. he doesn’t mind using it at all because it doesn’t sting or feel greasy. – Lily


Like many of you, our eczema journey is personal. That’s why we’re committed to creating a space for the eczema community to share experiences, be empowered through evidence-based solutions, and learn practical tips for daily life.
– Sajjad, Founder & CEO of NellaDerm

We noticed you're visiting from United States (US). We've updated our prices to United States (US) dollar for your shopping convenience. Use Canadian dollar instead. Dismiss