When to See a Dermatologist for Eczema: Red Flags You Shouldn’t Ignore
While some people can get by with over-the-counter creams and lifestyle tweaks, others find themselves in an exhausting cycle of flare-ups, sleepless nights, and worsening symptoms. So how do you know when it’s time to stop self-managing and start seeking professional help?

In this post, we break down exactly when to see a dermatologist for eczema, the red flags to watch for, and what a specialist can do that general care may miss.
Why Dermatologist Care Matters
Eczema (atopic dermatitis) is a complex, chronic inflammatory skin disorder. Its symptoms can range from mild dryness and irritation to painful, widespread inflammation that disrupts your quality of life.
Dermatologists are trained to:
- Diagnose different types of eczema
- Rule out look-alike conditions (like psoriasis or fungal infections)
- Prescribe advanced therapies beyond what you can buy at the pharmacy
- Manage complications like infections or contact allergies
Ignoring symptoms or relying solely on drugstore remedies for too long can delay proper treatment and even lead to skin damage or infections.
A peer-reviewed study in JAMA Dermatology found that early referral to a dermatologist can improve long-term eczema outcomes and reduce the risk of complications, including skin infections and steroid overuse (Silverberg et al., 2021).
Red Flags That Mean It’s Time to See a Dermatologist
If you’re experiencing any of the following, it’s time to book an appointment.
1. Your Eczema Isn’t Responding to Over-the-Counter Treatments
If you’ve tried moisturizers, 1% hydrocortisone creams, or antihistamines and your eczema persists for more than 2–3 weeks, it may require prescription-strength intervention.
This is especially true if the rash is:
- Spreading
- Becoming more inflamed
- Intensely itchy or painful
Delaying care may worsen your skin barrier dysfunction and make treatment harder down the line.
2. Your Symptoms Are Affecting Your Sleep, Work, or Mental Health
Eczema can be more than skin-deep. Studies show it’s linked to increased rates of anxiety, depression, and sleep disorders, particularly during severe flares.
If your eczema is:
- Keeping you awake at night
- Interfering with concentration or productivity
- Causing distress, embarrassment, or social withdrawal
…it’s time to talk to a dermatologist. Your mental health and quality of life matter as much as your skin.
3. You See Signs of Infection
When the skin barrier is broken or raw, bacteria like Staphylococcus aureus can enter and cause infection.
Warning signs include:
- Yellow or honey-colored crusts on the skin
- Oozing or pus
- Increased redness, warmth, and swelling
- Fever (in severe cases)
An infected eczema patch should never be ignored. Dermatologists can prescribe topical or oral antibiotics and help prevent recurring infections through targeted eczema control.
4. You’re Using Topical Steroids Frequently Without Improvement
Low- and mid-potency topical corticosteroids are often prescribed for flares—but long-term or incorrect use can cause:
- Skin thinning
- Stretch marks
- Topical steroid withdrawal (aka “red skin syndrome”)
If you find yourself relying on steroids too often, or needing stronger ones for results, your treatment plan needs reevaluation. A dermatologist can adjust your approach and possibly suggest alternatives like calcineurin inhibitors or biologic therapies.
5. You Suspect Allergies or Triggers You Can’t Identify
Sometimes eczema flares are driven by contact allergens—ingredients in cosmetics, fabrics, detergents, or even foods.
Dermatologists can perform patch testing to identify delayed-type allergies and help you eliminate hidden irritants that could be sabotaging your skin.
For more about identifying triggers, read 7 Eczema Triggers You Might Be Overlooking.
6. Your Eczema Covers a Large Area of Your Body
Mild eczema might stay confined to the hands, neck, or behind the knees. But widespread eczema across your limbs, trunk, or face requires medical attention—especially if it:
- Worsens rapidly
- Involves raw, open skin
- Affects your ability to wear clothing or function normally
Systemic treatments or light therapy (phototherapy) may be needed, and these require a dermatologist’s oversight.
7. You’re Pregnant or Have a Complicated Medical History
During pregnancy or in the presence of other conditions (like asthma or autoimmune disorders), eczema management becomes more complex. Certain medications are off-limits, and immune shifts can change how your eczema behaves.
A dermatologist can:
- Recommend pregnancy-safe treatments
- Coordinate care with your OB/GYN or other specialists
- Ensure eczema control without putting your health or baby at risk
The Eczema-Immune System Connection: Why Specialist Knowledge is Key
Eczema is fundamentally an immune-mediated disease. This chronic inflammation is not just a surface-level problem; it’s a breakdown in the skin’s defense mechanisms. The outer layer of skin, called the skin barrier, is compromised in eczema patients, allowing moisture to escape and irritants, allergens, and microbes to enter more easily. This triggers an overactive immune response, leading to the characteristic cycle of itching, scratching, and inflammation.
A dermatologist understands this intricate mechanism far beyond general medical practitioners. They don’t just treat the rash; they work to reset the underlying immune dysregulation and repair the damaged skin barrier. Understanding this complexity is critical because it explains why aggressive moisturizing alone often fails for severe cases. The professional goal is to suppress the excessive immune signals while simultaneously rebuilding the skin’s protective structure to reduce future flares.
Key aspects of the immune connection a dermatologist addresses include:
- T-helper cell activity: Specific immune cells (Th2 cells) release inflammatory proteins, or cytokines, that drive the redness and itch. Modern treatments, especially biologics, specifically target these pathways.
- Filaggrin deficiency: Many people with eczema have genetic mutations in the filaggrin gene, a protein vital for skin barrier formation. A dermatologist takes this genetic predisposition into account when recommending barrier-repairing topicals and moisturizers.
- The itch-scratch cycle: The intense itch is driven by inflammatory mediators (like IL-4, IL-13, and histamine). Scratching further damages the barrier, leading to more inflammation and infection risk. Breaking this cycle is a primary focus of prescription therapies.
The Spectrum of Advanced Eczema Treatments Only a Specialist Can Offer
When over-the-counter options fail, a dermatologist can unlock a comprehensive toolkit of advanced treatments, moving from topical prescriptions to systemic and light therapies. Knowing these options exist is a key reason when to see a dermatologist for eczema should be sooner rather than later.
Prescription Topical Medications
Beyond high-potency topical steroids, which are used carefully for short periods, a dermatologist can prescribe newer, non-steroidal options:
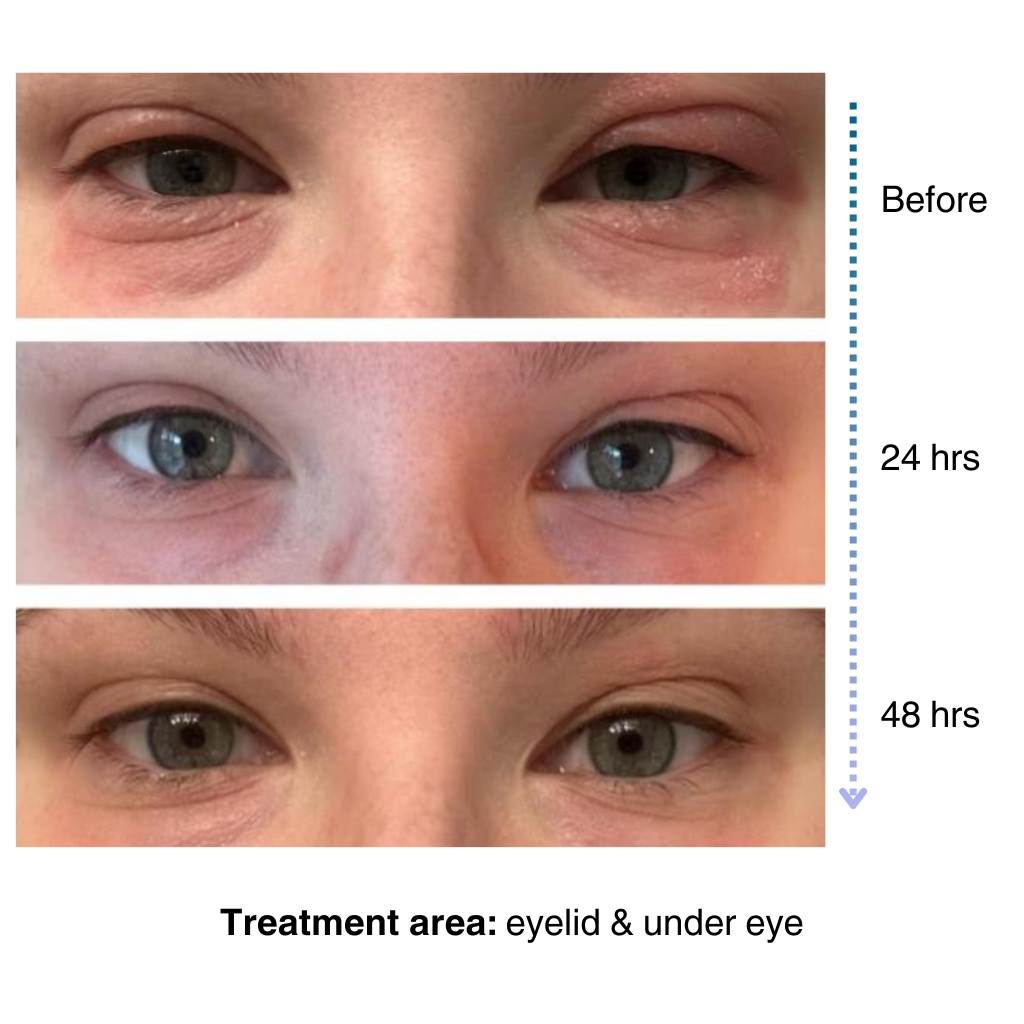
- Topical Calcineurin Inhibitors (TCIs): Medications like tacrolimus and pimecrolimus work by inhibiting the immune cells that cause inflammation. They are excellent for sensitive areas like the face and eyelids and do not carry the risk of skin thinning associated with prolonged steroid use.
- Topical PDE4 Inhibitors: Crisaborole is an example that works by blocking an enzyme in skin cells that contributes to inflammation, offering another non-steroidal option for mild-to-moderate eczema.
- Topical JAK Inhibitors: These are a newer class of topical treatments, like ruxolitinib, that block a signaling pathway inside immune cells, providing targeted relief for localized flares without impacting the entire body.
Phototherapy (Light Therapy)
For moderate to severe eczema that is widespread and hasn’t responded to topical treatments, phototherapy, or light therapy, is a highly effective, non-drug option administered in the dermatologist’s office.
- Narrowband Ultraviolet B (NB-UVB): This is the most common and safest form of phototherapy. It uses a specific wavelength of UV light to suppress the immune cells in the skin that cause inflammation and itch. Treatments are typically done 2-3 times per week for several months.
- How it works: The light energy modulates the immune response and can also help increase the body’s natural production of vitamin D, which is linked to better skin barrier function.
Systemic Therapies and Biologics
These treatments affect the whole body and are reserved for the most severe cases that have failed to respond to topical and light treatments.
- Oral Immunosuppressants: Older systemic drugs like cyclosporine or methotrexate can provide relief but require close monitoring due to potential side effects on the liver or kidneys. They are often used as a bridge treatment while waiting for biologics to take effect.
- Biologics: These are cutting-edge medications that target the precise immune molecules (cytokines) that drive eczema inflammation. This highly targeted approach means fewer side effects than traditional oral immunosuppressants.
Dermatologist Expertise: Ruling Out Look-Alike Conditions (The Diagnostic Imperative)
One of the most critical reasons when to see a dermatologist for eczema is necessary is to ensure you actually have eczema. Many other skin conditions can mimic the look and feel of atopic dermatitis, and treating the wrong condition can be ineffective or even harmful.
Conditions frequently mistaken for eczema include:
- Contact Dermatitis (Allergic and Irritant): While allergic contact dermatitis can co-exist with atopic dermatitis (eczema), the treatment is different. The primary focus is identifying and eliminating the specific trigger (like nickel, fragrances, or latex). A dermatologist uses patch testing to pinpoint these culprits, which is a specialized diagnostic skill.
- Psoriasis: Often confused with eczema due to redness and scaling, psoriasis is a different autoimmune disease. Eczema typically appears in skin creases (like the elbows and knees), while psoriasis often appears on the outside of joints. Treatments for psoriasis (like Vitamin D analogs) are often ineffective for eczema and vice versa.
- Fungal Infections (Tinea): Ringworm and other fungal infections can look like an eczema patch. Treating a fungal infection with a steroid cream (a common eczema treatment) can actually make the fungus proliferate, worsening the condition. A dermatologist can perform a simple skin scraping (KOH prep) to confirm a fungal diagnosis quickly.
- Seborrheic Dermatitis: This is common on the scalp, face, and chest and is often called “cradle cap” in infants. While it involves inflammation, it’s related to yeast overgrowth and requires anti-fungal shampoos and specific low-potency steroids, not the intensive moisture regimen of atopic dermatitis.
A dermatologist’s ability to accurately diagnose is the foundation of an effective treatment plan, saving the patient months or even years of ineffective self-treatment.
Optimizing Your Eczema Management: Beyond Medication and Topicals
While prescription treatments are vital for controlling flares, long-term eczema success relies on a holistic management plan, which a dermatologist helps you build. This plan includes precise guidance on lifestyle factors and the daily routine.
The Importance of Proper Moisturizing Technique
Moisturizing is often viewed as a simple step, but a dermatologist refines this into a crucial medical technique:
- The “Soak and Seal” Method: This involves a brief, lukewarm bath to rehydrate the skin, followed immediately (within three minutes) by applying prescription medication to inflamed areas and a thick emollient all over the body to lock in the moisture. This technique is often the difference between struggling and maintaining clear skin.
- Choosing the Right Emollient: Not all moisturizers are created equal. Dermatologists recommend thick ointments or creams over lotions, which contain more water and less oil. They also advise on products free of common irritants like fragrances, dyes, and lanolin, especially for those with sensitive skin.
Dietary Considerations and Eczema
The link between diet and eczema is complex and highly individualized. While routine elimination diets are generally discouraged, a dermatologist may recommend testing or consultation if a patient strongly suspects a food trigger, especially in young children.
- Focus on Anti-Inflammatory Foods: While not a cure, a diet rich in omega-3 fatty acids (found in fish), probiotics, and antioxidants can support overall skin health and reduce systemic inflammation.
- Identifying True Allergies: It is rare for a food allergy to be the sole cause of adult eczema, but true IgE-mediated food allergies can trigger immediate and severe flares. A dermatologist or allergist can perform blood or skin prick tests to differentiate between sensitivities and true allergies.
Climate and Environmental Adjustments
Environmental factors play a huge role in eczema severity. A dermatologist will discuss:
- Humidity Management: Dry air (often from central heating or winter weather) can strip the skin of moisture. A humidifier in the bedroom can be a low-cost, effective intervention.
- Clothing Choices: Coarse fabrics like wool can physically irritate the skin. Soft, breathable natural fibers like 100% cotton are almost always recommended to minimize friction and prevent overheating, a common trigger.
- Exercise and Sweat: Sweat contains salts that can sting and irritate raw eczema patches. A dermatologist will advise on strategies like showering immediately after exercise, even if it’s a quick rinse, and applying a thin layer of moisturizer or barrier cream before activity.
Eczema Across the Lifespan: Unique Considerations for Different Ages
Eczema presents differently depending on the age of the patient. A dermatologist tailors the diagnostic and treatment approach based on these differences, which is a major factor in when to see a dermatologist for eczema at a specific stage of life.
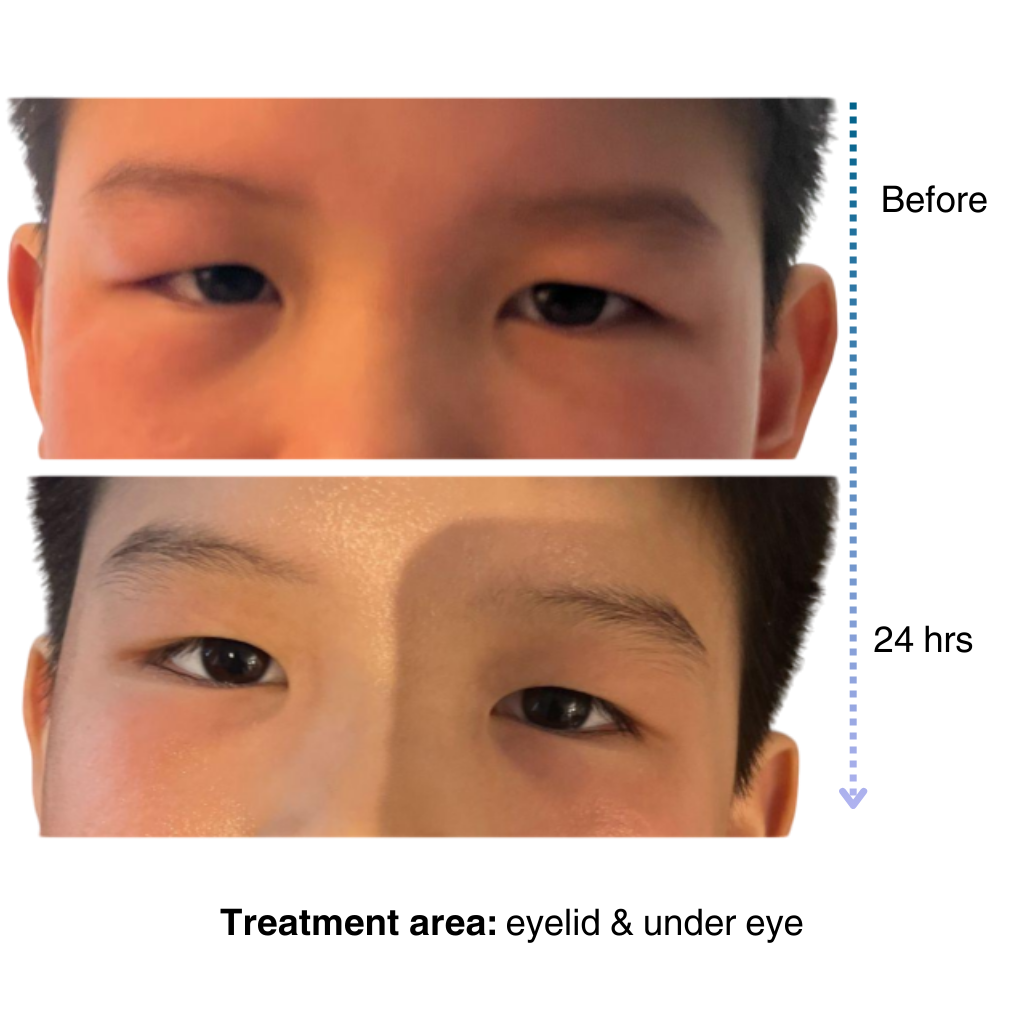
Infantile Eczema (Under 2 years old)
In infants, eczema often appears as crusty, weeping lesions, commonly on the face, scalp, and extensor surfaces (the outside) of the arms and legs.
- Key Management: Treatment heavily emphasizes diligent moisturizing and identifying potential food triggers (which are more common in this age group than in adults). Steroid use is typically low-potency and short-term due to the higher surface area to volume ratio in babies.
- Dermatologist Role: To distinguish eczema from seborrheic dermatitis (cradle cap) and ensure parents are not inadvertently causing harm with incorrect product application or excessive bathing.
Childhood Eczema (Ages 2 to Puberty)
The rash typically shifts to the flexural surfaces (the bends of the elbows and knees) and wrists, ankles, and neck. The patches become thicker and more leathery due to chronic scratching (lichenification).
- Key Management: Focus shifts to managing school-related stress, preventing infection (from scratching), and using prescription topicals. Phototherapy becomes an option for older children.
- Dermatologist Role: To educate the child and family on self-management techniques and determine if the child is a candidate for biologics or other advanced therapies if the disease is severe.
Adult Eczema
In adults, eczema may localize to specific areas, such as the hands (hand dermatitis), eyelids, or genitals. Stress and environmental/occupational triggers (like chemicals or solvents) become more prominent causes of flares.
- Key Management: Patch testing for contact allergies becomes critical, as does systemic treatment for widespread disease that impacts work and relationships.
- Dermatologist Role: To investigate occupational factors and manage the complex intersection of eczema with other chronic conditions (like hypertension or cardiovascular disease) which may influence systemic treatment choices.
The Hidden Costs of Delaying Eczema Care
While some people hesitate to see a specialist due to the perceived cost or time commitment, the long-term impact of untreated or poorly controlled eczema often leads to greater financial, physical, and emotional burdens. Understanding these hidden costs further emphasizes when to see a dermatologist for eczema should be a priority.
Increased Risk of Complications
- Skin Infections: Chronic scratching leads to breaks in the skin, increasing the risk of bacterial infections (like cellulitis) that require urgent care or hospitalization, incurring significant medical bills.
- Eczema Herpeticum: A rare but serious complication where the herpes virus infects the eczema-damaged skin. This is a dermatological emergency and requires immediate antiviral treatment.
- Lichen Simplex Chronicus: The thickening and darkening of the skin from habitual scratching. This cosmetic change is challenging to reverse and requires intensive, long-term care.
Socioeconomic and Quality of Life Impact
- Productivity Loss: Severe eczema leads to missed school days, reduced concentration at work, and diminished overall productivity due to pain, itching, and poor sleep quality. This loss of productivity can have a significant financial impact.
- Mental Health Strain: The chronic nature of the disease is a major driver of anxiety and depression. The cost of managing these secondary mental health issues (therapy, psychotropic medications) must be considered part of the overall disease burden.
- Cost of Ineffective Treatments: Patients often spend hundreds or thousands of dollars on unproven, alternative, or over-the-counter products in a desperate attempt to find relief. A dermatologist provides a clear, evidence-based treatment path, minimizing wasted expenditure on ineffective remedies.
What to Expect During a Dermatology Visit
Seeing a dermatologist for eczema isn’t just about getting stronger creams. A good appointment will include:
- Skin exam: To assess type, severity, and signs of infection
- History review: Previous treatments, triggers, allergies, family history
- Testing: May include patch testing, biopsies, or skin cultures
- Treatment planning: Prescription medications, lifestyle guidance, follow-up schedule
It’s helpful to bring:
- A list of all products you’re using (with photos or ingredient lists)
- Pictures of past flares
- A diary of recent flare-ups and possible triggers
Are Biologics an Option?
In cases of moderate-to-severe atopic dermatitis, dermatologists may prescribe biologic medications like Dupilumab (Dupixent). These target specific immune pathways and can dramatically reduce symptoms when topical treatments fall short.
Your dermatologist will determine if you’re a candidate based on:
- Severity and spread of eczema
- Response to past treatments
- Insurance coverage and medical history
Financial and Access Considerations for Eczema Care
The prospect of specialized care can be daunting, but there are resources available that your dermatologist’s office can often help you navigate. It is an important part of the conversation when deciding when to see a dermatologist for eczema.
Understanding Insurance Coverage and Assistance
Treatments for moderate-to-severe eczema, particularly biologics and phototherapy, can be expensive. A dermatologist’s office staff often has experience with insurance pre-authorizations and appeals, which are frequently required for systemic therapies. They can help you understand:
- Prior Authorization: The required documentation your insurance needs before approving a high-cost treatment.
- Patient Assistance Programs: Many pharmaceutical companies offer co-pay cards or assistance programs to help cover the out-of-pocket costs of biologics and other high-priced prescriptions. Your doctor’s office is the best source of information for these programs.
- Flexible Spending Accounts (FSA) and Health Savings Accounts (HSA): Dermatologist visits, prescription medications, and even some over-the-counter eczema treatments and humidifiers can be eligible for use with FSA/HSA funds.
Finding the Right Specialist
When looking for a dermatologist, consider:
- Specialization: Some dermatologists have a sub-specialty or a particular clinical interest in complex inflammatory skin diseases like atopic dermatitis. They may be more up-to-date on the newest research and treatment protocols.
- Pediatric Dermatology: If your child has eczema, a pediatric dermatologist is the ideal specialist, as they are trained to address the unique concerns of eczema management in infants and children.
- Telemedicine Options: For follow-up visits or for patients in rural areas, many dermatology practices now offer secure telemedicine appointments, which can make consistent care much more accessible.
The long-term cost of poorly controlled eczema, including missed work/school and repeated urgent care visits for infections, often outweighs the investment in specialized, proactive dermatological care.
When Your Skin Is Ready for a Reset
If your skin is overwhelmed, fragile, or constantly flaring, it may need more than moisturizers—it may need a full reset.
Pair your medical treatment with a clean, barrier-focused skincare routine. For flare-sensitive skin, NellaDerm’s NellaCalm offers gentle support that works alongside prescribed care without irritation. For daily maintenance, a hydrating cleanser helps preserve skin moisture without stripping essential lipids.
Final Thoughts
So, when should you see a dermatologist for eczema?
The short answer: As soon as your symptoms stop being manageable on your own.
Whether you’re battling stubborn flare-ups, potential infection, or emotional distress from chronic itching, dermatologists offer targeted, long-term solutions that go beyond temporary relief.
Don’t wait for your eczema to spiral out of control. The earlier you seek help, the better your chances of preventing complications and finding a treatment plan that truly works for you.